Invisible Disabilities Week
Invisible Disabilities Week is to help educate people that most disabilities are not obvious. Around 80% of people diagnosed with disabilities don’t have visible symptoms. The stigma we come across includes society, medical professionals, friends and family. There is still not enough funding to ensure these illnesses have treatment, a pathway and the right awareness.
Just a few Invisible Disabilities include:
Endometriosis
Functional Neurological Disorder
Myalgic Encephalitis
Fibromyalgia
Lupus
Multiple Sclerosis
Migraines
ADHD
You can find out more about the Sunflower lanyard and more information about invisible disabilities here: https://hdsunflower.com/uk/insights/category/invisible-disabilities
The Cost of Being Heard: Chronic Illness, Academia, and Black Women's Labour
A note from the author: What follows is both personal reflection and research insight—my experience of completing a PhD exploring Black undergraduate students' experiences in UK higher education whilst managing chronic illness, and what this dual reality revealed about institutional labour and care.
Sarah Gordon
As I approached the end of my PhD journey, I was often met with platitudes of strength, bravery, and resilience. As wonderful as it is to be recognised and appreciated, this also highlighted an uncomfortable shadow overpowering my experience. I began to understand why these words fell short, as this was not a show of individual resilience and strength. This was about systemic extraction of labour.
Throughout this period of my life, I was caught in a double bind. Experiencing major health complications and lifelong chronic illness diagnoses, whilst simultaneously trying to bring light to the injustices that academia perpetuates. But this is not unique to my experience. It is the reality for countless Black women navigating institutions that demand our labour whilst undermining our wellbeing.
The weight of invisible labour
This labour has a specific texture to it. It is the extra meeting where you explain (again) why being the only Black person in the room affects your participation. It is the emotional management required when academia dismisses your perspective. It is drafting and redrafting emails, editing your speech, calculating how much truth you can tell without being labelled "aggressive" or "difficult". It is having to justify why a racist incident was “actually” racist, whilst the person who caused harm remains comfortable.
It is not only my research that highlights student’s fatigue from repeatedly explaining racism and racialised experiences to uncomprehending staff (Arday 2018; Gordon, 2025). This is not an occasional frustration. It is an ongoing tax on their existence within the university. A communication gap between students and institutional representatives creating an additional psychological burden (Gordon, 2025). A burden that compounded the very struggles students were trying to articulate.
When your body says no: Chronic illness as consequence and complication
This work is often unpaid, unrecognised, and actively harms the people performing it. But here is what institutions refuse to acknowledge: this labour does not just exhaust us emotionally; it contributes deleteriously to our physical health. So, what happens when your body says no?
Audre Lorde knew this intimately. Writing whilst navigating cancer, she asked: "I don't feel like being strong, but do I have a choice?" (Lorde, 2020, p. 5). It is a question I found myself resonating with as my own health declined during my PhD. Our bodies are reverent archivists, unselective and not driven to please. The chronic stress of this labour, the constant vigilance, the emotional regulation, the exhaustion of being unheard, does not simply disappear. I felt this stress accumulate, lodging itself in my body. Research indicates the cumulative impact of navigating racist environments creates ongoing psychological burdens (Gordon, 2025). My experience taught me the harm extends far beyond the psychological. But having chronic illness does not exempt you from this labour, it compounds it. Now you are explaining racism and justifying accommodation needs. Now you are managing your symptoms and managing others' discomfort with your limitations. And through it all, you are expected to be strong.
The strength myth and its cost
The expectation of strength, often placed on Black women in academia, at times felt like an oppressive force rather than a source of empowerment (Gordon, 2025). This myth serves institutions, not us. It means our pain is minimised, our needs are questioned, and our exhaustion is reframed as inspiration. "You are so strong!" becomes another extraction. We are not allowed to be vulnerable, unwell, or tired. Both my research participants and I knew this trap well (Gordon, 2025). The worry was not just about being seen as weak, it was about confirming stereotypes, about giving institutions ammunition to dismiss their legitimate concerns about racism. This is what the strength myth costs us. We become palatable through our pain, inspirational through our endurance, valuable only as far as we can continue producing despite impossible conditions. We are expected to mentor junior students, educate resistant colleagues, sit on EDI committees, and perform "resilience" whilst our bodies are breaking down.
For many Black women in academia, strength is not a choice. It is a survival strategy in institutions that mistake our endurance for consent.
What institutions owe us - beyond Black History Month.
Black History Month often asks us to reflect on these concepts of resilience and strength. But this annual recognition rings hollow when institutions still expect us to perform that same resilience daily, without addressing the systems causing harm. So, what do institutions owe us? Not workshops we must run. Not committees where we are the only ones naming racism. Not praise for our strength. Institutions owe us environments where Black women do not have to choose between our health and our work. Culturally responsive mental health support that acknowledges race-based trauma as real and damaging (Gordon, 2025). Genuine accommodations for chronic illness that do not require us to perform worthiness. Time and space to rest without justification. Lorde wrote about living beyond fear and turning fury into creative energy (Lorde, 2020, p. 8).
But that transformation should not be mandatory or rushed. Sometimes we need to simply be unwell, be tired, be done - without institutions extracting that as a teaching moment. Black History Month is not about celebrating our survival. It is about demanding the conditions where we can thrive.
References
Arday, J. 2018. Understanding mental health: What are the issues for Black and ethnic minority students at University? Social Sciences. 7(10).
Gordon, S.R. (2025). From design to dialogue: a design-informed study on the experiences of Black undergraduates in Higher Education. PhD thesis. University of Nottingham. *
Lorde, A. (2020). The Cancer Journals. 004 ed. London: Penguin Classics.
*Dr Sarah Gordon's thesis will be available open access 10th December 2025, via the University of Nottingham E-prints.
Black History Month 2025
Black History Month 2025 is being celebrated this October (1st-31st) and this year's theme is Standing Firm in Power and Pride. We’re looking at the significant role people have played in medicine.
There is a long list of names and some we may never hear about, their contributions include life-changing medication and procedures:
Daniel Hale Williams- Performed the first successful open-heart surgery.
Rebecca Lee Crumpler- First African-American woman to become a medical doctor in the U.S
James McCune Smith- First African-American to earn a medical degree in the U.S
Charles Drew- Revolutionized blood storage techniques
Henrietta Lacks- African-American woman whose cancer cells are the source of the HeLa cell line, the first immortalized human cell line and one of the most important cell lines in medical research.
Marilyn Gaston- Leading researcher on sickle cell disease and the first African-American woman to head a major federal agency when she was appointed Director of the Health Resources and Services Administration (HRSA) in 1990.
Solomon Fuller, MD- made significant contributions to the study of Alzheimer’s disease.
Kizzmekia Corbett: A viral immunologist who led the NIH team that developed the Moderna COVID-19 vaccine
There are many more names we will never get to celebrate due to inequality and anti-blackness, we still have a long way to go. Happy Black History Month.
Resources: https://medicine.uky.edu/news/black-figures-medical-history-2022-02-09t18-20-25
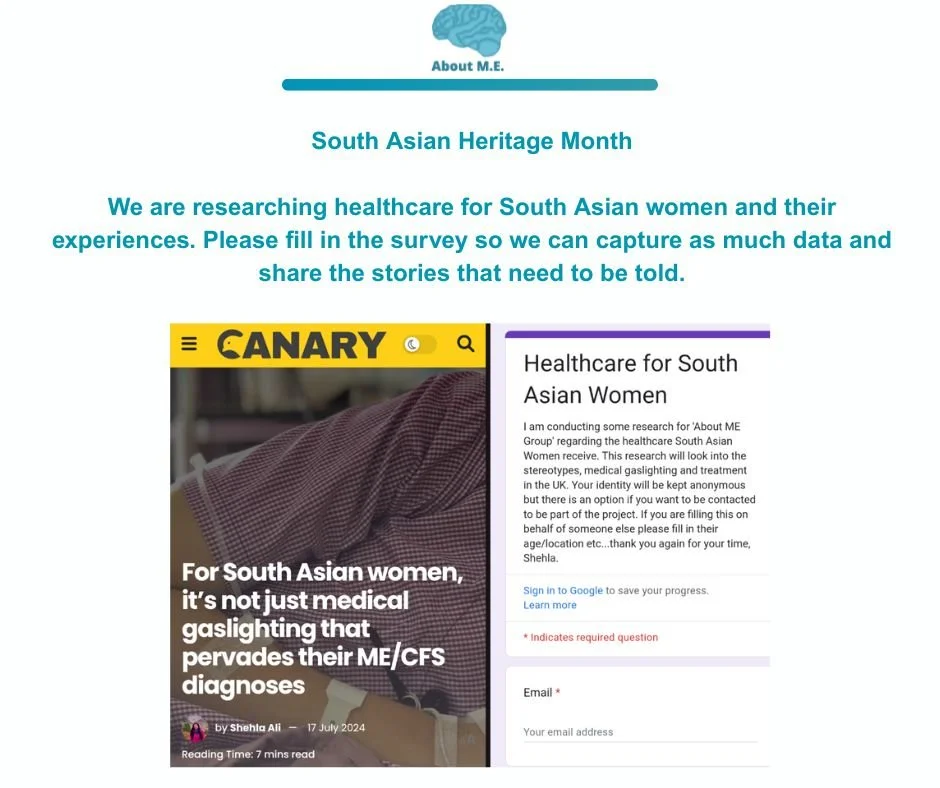
South Asian Women: Medical Bias
We are researching South Asian women's healthcare experiences and would appreciate it if you can fill in the survey or share please. Unfortunately it is a topic that is overlooked and we would like to share these stories as challenging as they might be.
Link to survey: https://bit.ly/HealthcareForSouthAsianWomen
Thank you.
Welfare Cuts are Deadly
The government have proposed that everyone already claiming PIP (Personal Independence Payment) will remain on the existing plan. Any new claimants will face a tougher criteria. Scope report that on an average households with a disabled person cost an additional £1,095 a month. Universal Credit is being cut and potentially frozen in certain areas. It said an estimated 150,000 people may be pushed into relative poverty by 2030 as a result of the welfare cuts. We believe these cuts will have a detrimental impact on people. We do not want to hear about well wishes and how the government think a forcing people into work will make people feel positive.
Please write to your MP asking them to say no to welfare cuts:
https://campaigns.scope.org.uk/page/172856/action/1?ea.tracking.id=website
Resources: https://assets.publishing.service.gov.uk/media/67e667fe4a226ab6c41b1fe2/spring-statement-2025-health-and-disability-benefit-reforms-impacts.pdf
Boundaries & Chronic Illnesses
Setting and maintaining boundaries when living with a chronic illness is essential for both your physical health and mental well-being. These boundaries help protect your spoons and can help create realistic expectations in relationships, work, and daily life. So let’s explore a few of these together.
1. Physical Boundaries
These are about managing your spoons, pain, and overall health.
Rest and Recovery: Say no to activities when your body needs rest—even if it's inconvenient for others.
Pacing: Break tasks into manageable parts and avoid overcommitting.
Diet and Medication: Stick to what your body needs even if others encourage otherwise, it is your body. There is also a lot of misinformation out there.
2. Emotional Boundaries
Protecting your emotional space is vital when others may not understand your illness.
Educate selectively: You don’t owe everyone a detailed explanation of your condition.
Limit toxic interactions: Avoid people who minimize or invalidate your experience (“But you were ok the other day”).
Permission to feel: Give yourself space to grieve, be angry, or rest without guilt.
3. Social Boundaries
Balance connection with self-preservation.
Decline without guilt: It’s okay to skip events or leave early if needed.
Flexible communication: Let friends know you might not always respond quickly or be available.
Selective sharing: Choose who you open up to and how much you disclose.
4. Work/Professional Boundaries
Navigating work with a chronic illness requires honest limits.
Disclosure (if appropriate): You can choose to inform your employer or HR for accommodations.
Reasonable accommodations: Ask for modified hours, remote work, or task adjustments.
Know your rights: In many places, disability protections exist i.e the UK.
5. Mental Health Boundaries
Living with chronic illness often impacts mental health, so set boundaries for psychological safety.
Therapy or support groups: A space where your experience is understood and validated.
Mental rest: Say no to emotionally taxing conversations or media that drain you.
Avoid over-researching: Protect yourself from overwhelm and misinformation online.
6. Internal Boundaries
Sometimes, the hardest person to set boundaries with is yourself.
Release unrealistic expectations: You don’t have to “push through” every time.
Self-talk check: Replace guilt or shame with compassion and acknowledgment.
Celebrate small wins: Honor what you can do, not just what you can’t.
Statement Regarding Palestine Action
We were born out of frustration of not being heard through systematic racism, medical trauma and dismissal. We are deeply concerned about the ban of Palestine Action UK, a movement that is trying to prevent war crimes. As soon as you begin criminalisation of freedom of speech and fundamental rights then you know it will continue within other movements. Humanitarian groups have asked for the aid blockade to stop with no changes.
We find ourselves facing a system and government investing in war crimes whilst making detrimental cuts to disability benefits and leaving those already vulnerable in dire conditions.
We stand with those risking their freedom to stop the ethnically cleansing of Palestinians.
Free Palestine.
Global Accessibility Awareness Day
Global Accessibility Awareness Day (GAAD), celebrated annually on the third Thursday of May, is a powerful opportunity to raise awareness and drive action on digital access and inclusion. It can help with:
1. Promoting Digital Inclusion
Encourages companies, governments, and individuals to ensure websites, apps, and digital tools are usable by everyone, including people with disabilities.
Highlights the importance of accessible design in everyday digital experiences.
2. Raising Awareness
Educates people about the barriers faced by individuals with visual, auditory, motor, and cognitive disabilities.
Brings attention to the importance of assistive technologies like screen readers, alternative input devices, and captioning tools.
3. Driving Innovation
Inspires developers, designers, and product teams to create inclusive solutions.
Promotes universal design principles that benefit all users, not just those with disabilities.
4. Encouraging Policy and Practice Changes
Motivates organizations to adopt accessibility standards (e.g., WCAG 2.1).
Spurs updates to internal processes, procurement policies, and compliance protocols.
5. Fostering Empathy and Understanding
Provides real-life examples and simulations to help people understand what accessibility challenges feel like.
Promotes storytelling from disabled voices to humanize digital barriers.
6. Supporting Workforce Inclusion
Encourages inclusive hiring practices and accessible workplace tools.
Raises awareness about the importance of accessible training materials and job platforms.
International ME/Fibromyalgia Awareness Day
May 12 is observed worldwide as International ME/ Fibromyalgia Awareness Day. It's a time to recognize and support people living with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia, two often misunderstood and debilitating chronic illnesses that significantly impact quality of life.
💜 Raising Awareness on May 12
Wearing blue or purple, sharing stories online, lighting landmarks, and supporting advocacy organizations can help bring visibility to these often invisible illnesses.
💡 What Is Fibromyalgia?
Fibromyalgia is a chronic condition characterized by:
Widespread musculoskeletal pain
Extreme fatigue
Sleep disturbances
Cognitive issues ("fibro fog")
Sensitivity to touch, light, sound, or temperature
While the exact cause is unknown, it's believed to involve abnormal pain processing in the brain and nervous system. It often co-occurs with ME/CFS, which shares overlapping symptoms.
💙 How to Deal with Fibromyalgia
Managing fibromyalgia is a multifaceted approach. There's no cure, but symptoms can often be managed with a combination of strategies.
ME/CFS stands for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. It is a serious, long-term illness that affects multiple systems in the body, especially the nervous, immune, and energy metabolism systems. Here's a breakdown of what it involves:
Core Features:
Persistent, unexplained fatigue: Not improved by rest and significantly worsened by physical or mental activity.
Post-exertional malaise (PEM): A hallmark symptom where symptoms dramatically worsen after even minor exertion.
Unrefreshing sleep: Despite sleeping for long periods, patients wake up feeling tired or unrested.
Cognitive impairments: Often described as "brain fog"—problems with memory, focus, and processing information.
Orthostatic intolerance: Difficulty standing or sitting upright for long periods due to issues with blood pressure or heart rate regulation.
Additional Symptoms May Include:
Muscle or joint pain
Headaches
Sensitivities to light, sound, or chemicals
Digestive issues
Sore throat or swollen lymph nodes
Diagnosis:
There is no single test for ME/CFS. Diagnosis is based on:
Symptoms lasting at least 6 months
Ruling out other possible causes
Meeting clinical criteria
There is no cure, and treatments focus on symptom management:
Sensory Challenges and Events
Attending events with sensory issues due to a chronic illness can be overwhelming, but with the right strategies, it can become more manageable. Here are some common challenges and tips for handling them:
Common Sensory Challenges
Noise Sensitivity – Loud music, crowds, and overlapping conversations can be overstimulating.
Light Sensitivity – Bright lights, flashing lights, or screen glare may cause discomfort or migraines.
Temperature Sensitivity – Some chronic conditions make it hard to regulate body temperature.
Touch Sensitivity – Crowded spaces, tight seating, or certain fabrics can trigger discomfort.
Smell Sensitivity – Strong scents (perfumes, food, cleaning supplies) can cause nausea or headaches.
Tips for Managing Sensory Overload at Events
Plan Ahead
Choose quieter times to attend (e.g., early in the day or on weekdays).
Check if the venue has accommodations (quiet areas, seating options, sensory-friendly spaces).
Call ahead to ask about strobe lights, music levels, or fragrance-free policies.
Bring Sensory Aids
Earplugs or Noise-Canceling Headphones – Reduce overwhelming sounds.
Sunglasses or Tinted Glasses – Help with bright lighting or screen glare.
Comfortable Clothing – Soft, breathable fabrics and layers to adjust for temperature changes.
Essential Oils or Face Masks – Help block out strong odors.
Have an Exit Plan
Identify quiet spots or places to take breaks.
Park close to the entrance/exit if possible.
Go with someone who understands your needs and can help if you need to leave.
Communicate Your Needs
Let a friend, family member, or event staff know if you need accommodations.
Use a medical alert bracelet or card if necessary.
Take Care of Your Body
Stay hydrated and bring snacks if needed.
Rest before and after the event to prevent overstimulation.
Listen to your body and leave if symptoms worsen.
Why Chronic Illnesses Can Be Difficult To Recognise
Subtle and Varied Symptoms:
Chronic illnesses often have symptoms that are not immediately obvious or visible, which can lead to delays in getting a diagnosis.
Overlapping Symptoms:
Many chronic illnesses share common symptoms, making it difficult to pinpoint the underlying cause. For example, fatigue, pain, and digestive issues can be associated with various conditions.
Long Latency Periods:
The time between the onset of a chronic illness and the appearance of noticeable symptoms can be long, further complicating early detection.
Lack of Specific Tests:
Some chronic illnesses lack specific diagnostic tests, making it challenging for healthcare providers to confirm a diagnosis.
Psychological and Social Factors:
The emotional and social impact of chronic illness can also be significant, potentially leading to difficulties in recognizing and coping with the condition.
Fatigue:
Chronic illnesses can cause significant fatigue, which can be a major symptom that is often overlooked or misattributed to other causes.
Impact on Daily Life:
Chronic illnesses can disrupt daily life, leading to difficulties with work, relationships, and social activities, which can further complicate recognition and management.
Mental Health:
Chronic illness can also impact mental health, leading to anxiety, stress, and depression, which can make it harder to recognize and cope with the physical symptoms.
FND Awareness Day
It was five years ago I became bedridden with unexplained symptoms. The year before, I was travelling around the world solo, running a business and working out at the gym. I didn’t think I would get sick, people with chronic illnesses rarely do. But it was one of the worst years of my life. A sense of confusion, not belonging, bitterness towards the world and hoping for it to all go away.
I am #FNDAware
I was diagnosed with FND Functional Neurological Disorder. A neurological condition, one that is still underfunded and misunderstood. A common way of describing FND is that the brain sends the wrong signals to the nervous system. Although the government has announced investing in FND, there is still a long way to go.
Remember your feelings are valid and you are allowed to mourn. Unfortunately, there is still a lot of ableism and people who have never heard of the illness who get to decide on treatment, or lack of.
One day at a time.
Adjusting to Living with a Chronic Illness
Adjusting to life with a chronic illness is a journey—one that comes with emotional, physical, and lifestyle changes. Here are a few tips to help navigate this change in your life:
1. Acknowledge Your Feelings
It's completely normal to experience grief, frustration, anger, or sadness. Give yourself permission to feel these emotions and seek support when needed. There may be things you used to love, whether that’s hobbies or work which you can no longer carry out.
2. Educate Yourself
Understanding your condition can help you to make informed decisions about your health. Read reputable sources, join support groups, and communicate openly with your healthcare providers.
3. Prioritize Self-Care
Physical Health: Follow your treatment plan, get adequate rest, and maintain a balanced diet.
Mental Health: Practice stress management techniques such as meditation, therapy, or journaling.
Pacing Yourself: Learn to listen to your body and avoid overexertion.
4. Build a Support System
Surround yourself with supportive friends, family, and professionals who understand your journey. Online communities and local support groups can be valuable resources.
5. Adapt Your Daily Life
Make adjustments to your work, home, and social life to accommodate your needs. This may include using assistive devices, modifying your workspace, or setting realistic goals.
6. Advocate for Yourself
Don’t hesitate to communicate your needs to employers, family, and healthcare providers. Setting boundaries and speaking up about what you require can improve your quality of life.
7. Focus on What You Can Control
Rather than dwelling on limitations, find joy in the things you can do. Engaging in hobbies, creative outlets, or new activities can bring a sense of purpose.
Chronic Illnesses & Ramadan
Ramadan & Chronic Illnesses
People with chronic illnesses can find it hard to participate in religious/cultural events, but that doesn’t make them any less as a person. With Ramadan beginning it’s a reminder that you don’t need to ask anyone whether or not they are fasting.
Ramadan is the holiest month in the Islamic calendar, observed by Muslims worldwide as a time of fasting, prayer, reflection, and community. The fast is broken with a meal called Iftar, traditionally starting with dates and water, followed by a larger meal. The pre-dawn meal before fasting begins is called Suhoor.
Who is Exempt from Fasting?
Certain people are exempt from fasting, including:
Children who have not reached puberty
The elderly and those with chronic illnesses
Pregnant and nursing women (if fasting is difficult)
Travellers
Menstruating women (they make up the missed fasts later)
What you can do instead?
Give to charity
Volunteer
Increase your knowledge
We recommend speaking to your doctor and local Imam about your circumstances and ask them for advice. You also know your body best.
Ramadan Mubarak to all.
Life After Gaza: Surviving, Advocating & Moving Forward
Gaza My Home
Living in Gaza is unlike anywhere else in the world. For over three decades, it was my home—my place of work, my community, and where I built my life. The challenges were constant, from power shortages to movement restrictions, but so was the resilience. Gaza is filled with talented, ambitious people who strive to create opportunities despite the odds. Working at Gaza Sky Geeks, I saw firsthand how young people used technology and freelancing to break past physical barriers and access global markets. Yet, no matter how much we achieved, the reality of the blockade always loomed over us, reminding us that our futures were never fully in our control.
Disabilities in Gaza
During the last war, I was responsible for over 45 immediate family members, including my three children and elderly parents. My father, who is in a wheelchair, requires constant care. We were displaced multiple times across the strip, and as the sole breadwinner, I had to provide shelter, food, water, and whatever necessities I could find. We survived over seven months of everything the world witnessed online, but then I had to make the hardest decision of my life: leaving Gaza. I wasn’t able to save everyone—only 10 out of the 45 family members I was responsible for made it out. A week later, the borders were completely closed.
I am one of the fortunate ones who managed to escape, but with that comes a burden I never anticipated: survivor’s guilt. Every day, I think of my family, friends, colleagues, and loved ones still trapped in impossible conditions. The guilt manifests in unexpected ways—hesitation before sharing good news, feeling like I don’t deserve a fresh start when others are suffering, and the relentless question of whether I am doing enough to help those left behind. I face waves of deep depression, weakness, and helplessness, struggling to find meaning in this new reality.
Image Credit: Saed Habib
Advocacy & Mental Health
Since leaving, I have taken on a new role: advocate. I use my voice to bring attention to Gaza’s ongoing struggles, especially in the tech and business sectors. I push for more opportunities for Palestinians in Gaza, the West Bank, and those displaced in Egypt and beyond. This advocacy work, however, takes a toll on my mental health. Every conversation about Gaza reopens wounds that have barely started to heal. The weight of carrying the stories of those who cannot speak for themselves is heavy, and burnout is a real concern.
One of the most powerful tools in advocacy today is social media. Platforms like Facebook, X, LinkedIn, and Instagram allow us to amplify Palestinian voices and counter misinformation. But the constant exposure to distressing images and news can be overwhelming. While social media is a lifeline for spreading awareness, it is also a double-edged sword, contributing to anxiety and emotional exhaustion. Balancing advocacy with self-care is an ongoing struggle—one I am still learning to navigate.
A topic that often gets overlooked in discussions about Gaza is the experience of people with disabilities. The war has dramatically increased the number of individuals with disabilities, whether from injuries, trauma, or lack of medical care. Even before the war, Gaza was a difficult place for people with disabilities, with limited accessibility and resources. Now, with infrastructure destroyed and medical aid restricted, their struggles are even more severe. Advocacy for Gaza must include them, ensuring that any rebuilding efforts are inclusive and that they are not left behind.
As for my own mental health, it is a work in progress. The trauma of war, displacement, and the uncertainty of what comes next weigh heavily on me. Some days, I am focused and driven, determined to make an impact. On other days, the sheer magnitude of loss feels paralyzing. Therapy is not always accessible, so I rely on community support, self-reflection, and advocacy as a form of healing. But healing is not linear, and I remind myself that it is okay to take things one step at a time.
Healing
So, what’s next for me? I am exploring different paths, from remote work to potential relocation opportunities. I am committed to continuing my advocacy, helping Palestinian professionals connect with global opportunities, and ensuring that Gaza’s story is not forgotten. My goal is to find a way to balance personal healing with meaningful work—work that not only supports my family but also contributes to a better future for my people.
For anyone reading this, especially those who have supported Gaza from afar: your voice matters. Your engagement matters. Whether through social media, donations, or policy advocacy, every action counts. Gaza is more than a conflict zone—it is home to people with dreams, talents, and limitless potential. And as long as we keep telling our stories, those dreams will not be forgotten.
Written by Saed Habib
A New Year, Same Chronic Illness
Navigating your mental health while managing a chronic illness can be particularly challenging but also deeply rewarding as you discover strategies that enhance your well-being. Here are some thoughtful ways to approach it in the new year, or you can completely ignore this article, we know how it is:
1. Set Realistic Goals
Prioritize Self-Compassion: Accept that your energy levels (spoons) and abilities may vary. Set flexible goals that accept your limits.
Focus on Small Wins: Celebrate even small achievements to maintain motivation and a sense of progress.
2. Build a Support Network
Connect with Others: Join support groups, either in-person or online, for people with similar conditions. Shared experiences can reduce feelings of isolation.
Lean on Loved Ones: Communicate openly with family and friends about your needs and feelings or not. If you feel triggered by opening up to people you know you can always find people who have similar illnesses and experiences.
3. Integrate Mindfulness Practices
Mindfulness Meditation: Regular practice can help reduce anxiety, depression, and pain sensitivity.
Deep Breathing Techniques: Useful during moments of stress or when dealing with symptoms.
4. Prioritize Therapy
Seek Professional Support: Therapists, particularly those specializing in chronic illness, can offer tools to navigate emotional challenges.
5. Cultivate a Routine
Balance Activity and Rest: Develop a routine that includes time for work, self-care, and leisure without overdoing it.
Sleep Hygiene: Maintain consistent sleep patterns to improve mood and energy levels. (we know this can be tricky)
6. Practice Gratitude
Journaling: Reflect on positive moments or things you’re thankful for each day.
Shift Focus: Recognizing small joys can help counterbalance the challenges of chronic illness.
7. Engage in Creative Outlets
Express Yourself: Writing, art, or music can be therapeutic and help process emotions.
Try Something New: Explore hobbies that align with your current abilities and interests. Or research a random topic that is interesting to you.
8. Stay Physically Active Within Your Limits
Adapted Exercise: Gentle movement like yoga, tai chi, or walking can boost endorphins and reduce stress. But if it means gentle exercises then do that, it’s all about what works for your body.
Physical Therapy: If applicable, consult a professional for safe exercises tailored to your condition.
9. Educate Yourself
Understand Your Condition: Knowledge can empower you to advocate for your needs and make informed decisions.
Learn Coping Strategies: Research tools and techniques that others with similar conditions have found helpful.
10. Plan for Challenges
Create a Safety Net: Identify triggers or difficult situations and have a plan to address them (e.g., relaxation techniques or reaching out for support).
Allow Flexibility: Be gentle with yourself if plans need to change due to your health.
11. Celebrate Progress
Acknowledge Growth: Look back at how far you’ve come, even if the journey is ongoing.
Reward Yourself: Treat yourself for milestones, no matter how small.
Navigating mental health alongside a chronic illness is an ongoing process. Take it one step at a time, and remember that seeking help is a sign of strength, not weakness. Starting the new year with a focus on self-care and intentionality can set a positive tone for the months ahead.
Why are Chronic Illnesses so Difficult to Understand
Chronic illnesses are difficult to understand for several reasons, mainly due to their complexity, variability, and often invisible nature. (Views expressed are personal). Here are some key reasons:
1. Complex
Chronic illnesses often affect multiple systems in the body, not just one organ or area. Conditions like M.E., Lupus, or Multiple Sclerosis have wide-ranging effects that can involve the immune system, cardiovascular system, and nervous system, among others. This makes it hard to pin down the full scope of the illness, as symptoms can manifest in unpredictable ways across different parts of the body.
2. Invisible Symptoms
Many chronic illnesses involve symptoms that are not visible or easily measurable. Pain, fatigue, or cognitive issues (brain fog) are difficult to quantify or observe from the outside. Blood tests and MRI Scans usually appear ‘clear’ which on paper will suggest the person is ‘healthy’. This invisibility can make it harder for others to understand the severity or even the reality of what the person is going through, leading to misconceptions about the illness.
3. Unpredictability and Fluctuations
Chronic illnesses often have fluctuating symptoms. People may have "good days" where they feel fine, followed by sudden "flare-ups" where symptoms worsen unexpectedly. This inconsistency can make the illness harder to track and understand, both for the individual and healthcare providers, and may lead to the belief that the illness isn’t as serious as it really is or to quote “in your head”.
4. Multiple Causes and Triggers
The causes of chronic illnesses are often multifactorial, involving genetics, environment, lifestyle, and sometimes unexplained factors. For example, autoimmune conditions like rheumatoid arthritis or Crohn’s disease may be triggered by a combination of genetic predisposition and environmental stressors, but pinpointing the exact causes or triggers can be challenging. This complexity can lead to confusion and difficulty in finding effective treatments. Someone can go from running marathons, eating fairly healthy and exercising to becoming bedridden.
5. Individualised Experiences
Every person with a chronic illness experiences it differently. Even people diagnosed with the same condition may have very different symptoms, treatment responses, and outcomes. For example, two people with fibromyalgia might report vastly different pain levels or fatigue, making it hard to generalize or create standardized treatment plans that work for everyone.
6. Psychosocial and Emotional Impact
Chronic illnesses can affect a person’s mental and emotional health, leading to anxiety, depression, or social isolation. These psychosocial aspects often intertwine with physical symptoms, making it harder to distinguish what is causing which symptom. The mind-body connection plays a significant role, adding another layer of complexity to understanding these conditions.
7. Evolving Understanding and Research
Medical science is still evolving when it comes to many chronic conditions. Conditions like chronic fatigue syndrome (CFS), fibromyalgia, or irritable bowel syndrome (IBS) were not fully acknowledged by the medical community until relatively recently. New discoveries are still being made about the underlying mechanisms of these conditions, which means our understanding is incomplete.
8. Difficulty in Diagnosis
Many chronic illnesses are difficult to diagnose, requiring numerous tests, specialists, and sometimes even trial-and-error treatments before a diagnosis is confirmed. Some conditions, like Lyme disease or lupus, may take years to diagnose because their symptoms overlap with other illnesses or are not immediately obvious. This diagnostic uncertainty adds to the difficulty in understanding the illness.
9. Chronic Nature and Lack of Cure
Since chronic illnesses are long-term and, in many cases, have no cure, managing them becomes a lifelong challenge. The uncertainty and long-term nature of the illness can make it emotionally and physically draining, not just for patients but also for family members and caregivers. This prolonged struggle complicates the understanding and management of the disease.
10. Stigma and Misunderstanding
Some chronic illnesses, particularly those that affect mental health or cognitive function (such as chronic pain conditions or autoimmune diseases), are often stigmatized or misunderstood by society. Patients may face skepticism or lack of empathy, which further complicates the understanding of their condition, both on a personal and societal level.
In short, chronic illnesses are difficult to understand because they are highly complex, can be invisible or fluctuating, affect individuals differently, and are often accompanied by emotional, psychological, and social challenges. This makes them both medically and socially difficult to grasp fully.
Managing chronic illnesses in a different season
Managing chronic illnesses in different seasons requires adapting self-care strategies to account for weather, environmental changes, and seasonal triggers. (***Disclaimer we are not medical experts, this article is opinion based***
Here's a breakdown of how to manage common chronic conditions across different seasons:
1. Respiratory Conditions (Asthma, COPD)
Winter:
Cold weather can constrict airways and worsen symptoms.
Tip: Wear a scarf or mask over your nose and mouth when outdoors to warm the air you breathe. Avoid outdoor exercise during cold weather, and use a humidifier indoors to reduce dry air.
Spring/Summer:
Allergens such as pollen can trigger symptoms.
Tip: Stay indoors on high-pollen days, keep windows closed, and use air purifiers. Medications like antihistamines or inhalers should be readily available.
2. Cardiovascular Conditions (Hypertension, Heart Disease)
Winter:
Cold weather causes blood vessels to constrict, raising blood pressure.
Tip: Dress warmly and avoid sudden exposure to the cold. Ensure regular monitoring of blood pressure.
Summer:
Heat can cause dehydration and make the heart work harder.
Tip: Stay hydrated, avoid excessive heat, and exercise during cooler parts of the day. Be cautious with diuretics, which can increase dehydration risk.
3. Diabetes
Winter:
Physical inactivity and comfort foods can affect blood sugar levels.
Tip: Maintain a regular exercise routine indoors, monitor your blood sugar levels more frequently, and avoid sugary comfort foods.
Summer:
Dehydration can affect blood glucose control.
Tip: Drink plenty of water, avoid prolonged exposure to heat, and store insulin properly (as extreme heat can reduce its effectiveness).
4. Rheumatoid Arthritis and Joint Pain
Winter:
Cold, damp weather can worsen joint stiffness and pain.
Tip: Keep joints warm, consider hydrotherapy, and stay physically active with indoor exercises like stretching or swimming.
Summer:
Heat can reduce stiffness but also lead to fatigue.
Tip: Engage in gentle outdoor activities in the early morning or evening to avoid overheating. Stay hydrated and cool.
5. Chronic Skin Conditions (Eczema, Psoriasis)
Winter:
Dry, cold air can exacerbate skin dryness and flare-ups.
Tip: Use heavy moisturizers, avoid hot showers, and run a humidifier indoors.
Summer:
Sun exposure can improve some conditions (e.g., psoriasis) but worsen others (e.g., eczema).
Tip: Use sunscreen, limit sun exposure, and avoid harsh soaps that can irritate sensitive skin.
6. Mental Health Conditions (Depression, Anxiety)
Winter:
Seasonal Affective Disorder (SAD) and less sunlight can worsen depression.
Tip: Use light therapy, take walks during daylight, and stay socially connected.
Summer:
Heat and long days may exacerbate anxiety or sleep disturbances.
Tip: Stick to regular sleep schedules, manage stress with meditation or breathing exercises, and avoid overstimulation.
7. Chronic Pain (Fibromyalgia)
Winter:
Cold weather may increase muscle stiffness and pain sensitivity.
Tip: Use warm baths, heating pads, and gentle stretching to alleviate discomfort.
Summer:
Fatigue can worsen in hot weather.
Tip: Rest during the hottest parts of the day, engage in light, low-impact activities like swimming, and stay hydrated.
General Tips Across Seasons:
Maintain medication adherence: Seasons don’t change the need for regular medication. Keep them stored properly in accordance with temperature guidelines.
Stay active: Adapt exercise routines to each season (indoor workouts during winter, early morning walks in summer).
Dietary Adjustments: Tailor meals to seasonal availability of fresh produce while considering your condition (e.g., heart-healthy diets in winter to manage cholesterol).
Regular check-ups: See your healthcare provider regularly, especially during seasonal changes when symptoms might flare up.
By adjusting lifestyle habits and routines, you can effectively manage chronic conditions through the challenges posed by each season.
World Mental Health Day
World Mental Health Day
World Mental Health Day, observed on October 10th each year, is an opportunity to raise awareness, promote mental health education, and advocate for mental health support. Dealing with this day can involve several meaningful actions for yourself and your community. This year’s theme is focusing on workplaces. For those with chronic/invisible illnesses it may feel irrelevant. It can also feel overwhelming seeing a number of posts about something you may have been battling for everyday. ***Disclaimer*** This is an opinion post, we are not medical professionals.
1. Self-Care and Reflection
Assess your mental health: Take time to check in with yourself emotionally, mentally, and physically. Use mindfulness techniques, journaling, or meditation to understand how you're feeling.
Practice self-care: Engage in activities that bring you peace and joy, such as exercise, reading, or spending time in nature.
Talk to someone: If you're feeling overwhelmed, reach out to a trusted friend, family member, or a mental health professional for support.
2. Educate and Raise Awareness
Learn about mental health: Take the opportunity to educate yourself about mental health conditions, available support systems, and ways to promote mental well-being.
Share resources: Use your social media platforms to share information, helplines, or personal stories about mental health. You can post infographics, articles, or videos that highlight the importance of mental health care.
Participate in discussions: Join webinars, community events, or panels that address mental health challenges and solutions, particularly those focused on stigma reduction and access to care.
3. Support Others
Check in on loved ones: Reach out to friends, family members, or colleagues to ask how they are doing. Sometimes, just letting someone know you care can make a big difference.
Volunteer or donate: Support mental health organizations through volunteering or by making a donation. You can also help by advocating for mental health policies in your community or workplace.
4. Advocate for Change
Promote mental health at work or school: Encourage your workplace or school to provide mental health resources, host workshops, or offer mental health days.
Advocate for policy changes: Support movements that push for increased funding for mental health services, improved access to mental health care, and anti-stigma campaigns.
Engage in mental health activism: Share your story (if comfortable) to break the silence around mental health and reduce stigma in your community.
5. Participate in Events
Join World Mental Health Day campaigns: Many organizations host events like walks, talks, workshops, and fundraisers. Participate in these activities to show solidarity and support.
Wear green: Green is the color for mental health awareness. Wearing green on World Mental Health Day can be a simple way to show support.
6. Seek Professional Help If Needed
If you're struggling with your mental health, use this day as a reminder to seek professional help. Therapy, counselling, or speaking with a mental health expert can be transformative.
Ideas to Celebrate:
Organize a virtual mental health workshop.
Take part in a local charity run or walk for mental health.
Create a calming space at home for mindfulness and relaxation.
World Mental Health Day is about spreading awareness, compassion, and understanding around mental health issues.
Preparing for an MRI
How to prepare for MRI Scans
Preparing for an MRI (Magnetic Resonance Imaging) scan can help ensure a smooth and successful procedure. Here’s what you can expect and how to prepare: ***Disclaimer*** We are not medical specialists and this is opinion based.
1. Before the Scan:
Follow Pre-Scan Instructions:
Your healthcare provider will give you specific instructions based on the type of MRI. These may include fasting (if contrast dye will be used) or avoiding certain medications.
Inform Medical Staff About Medical Conditions:
Let the radiologist know if you have any metal implants (like pacemakers, joint replacements, or metal plates), as these may interfere with the scan.
Mention any allergies, especially if a contrast dye will be used.
If you’re pregnant or suspect you might be, inform your doctor.
Claustrophobia or Anxiety:
If you're claustrophobic or anxious, let the staff know beforehand. They may offer sedation or allow you to bring calming aids like music. Or give you headphones and a blindfold.
2. Clothing and Personal Items:
Wear Comfortable, Loose-Fitting Clothes:
You might be asked to change into a hospital gown depending on the scan location and facility policies.
Remove Metal Objects:
This includes jewelry, watches, hairpins, eyeglasses, hearing aids, dentures, and any clothing with zippers or metal.
No Electronics:
Leave your phone, credit cards, or any electronic devices outside the scan room as the MRI's magnetic field can damage them.
3. During the Scan:
Stay Still:
The MRI machine takes detailed images, so it’s important to remain as still as possible. Any movement can affect the quality of the images.
Noise:
MRI machines are loud (buzzing, thumping, knocking sounds). You’ll be given earplugs or headphones to reduce the noise.
Length of Scan:
The scan can take anywhere from 15 minutes to over an hour, depending on the area being examined.
Communication:
You'll be in constant communication with the technician via a microphone. You can also alert them if you need to stop.
4. After the Scan:
If Contrast Dye Was Used:
You might be asked to drink extra fluids to help flush the dye from your system.
No Downtime Needed:
For most MRI scans, you can resume normal activities right after the procedure unless you’ve been sedated.
Tips:
Arrive early to fill out paperwork and ask any last-minute questions.
Bring someone to drive you home if you’re taking a sedative.
Preparing well will help you feel more comfortable during the MRI scan, and following these guidelines ensures a smoother process. However, we understand that not everyone has the same experiences.